
You begin with small delays, such as 30 minutes, and gradually work your way up to urinating every three to four hours. Bladder training involves training yourself to delay voiding when you feel an urge to urinate. Absorbent garments come in a variety of sizes and absorbency levels. Wearing absorbent pads or undergarments can protect your clothing and help you avoid embarrassing incidents, which means that you won't have to limit your activities. Ask your doctor if this approach is right for you. If you are not able to empty your bladder well, using a catheter periodically to empty your bladder completely helps your bladder do what it can't do by itself. Setting a schedule for toileting - for example, every two to four hours - gets you on track to urinate at the same times every day rather than waiting until you feel the urge to urinate. Weight loss may help if you also have stress urinary incontinence. If you're overweight, losing weight may ease symptoms.
#Post void residual icd 9 how to#
The biofeedback sensors teach you how to make subtle changes in your body, such as strengthening your pelvic muscles so that when you have feelings of urgency you're better able to suppress them. During biofeedback, you're connected to electrical sensors that help you measure and receive information about your body. Just like any other exercise routine, how well Kegel exercises work for you depends on whether you perform them regularly. Your doctor or a physical therapist can help you learn how to do Kegel exercises correctly. These strengthened muscles can help you stop the bladder's involuntary contractions. Kegel exercises strengthen your pelvic floor muscles and urinary sphincter. They're often effective, and they carry no side effects. Kegel exercises can help strengthen these muscles.īehavioral interventions are the first choice in helping manage an overactive bladder.

The male pelvic floor muscles support the bladder and bowel and affect sexual function. Your doctor will review the results of any tests with you and suggest a treatment strategy. This procedure can identify whether you have involuntary muscle contractions or a stiff bladder that's not able to store urine under low pressure. The sensor tells how much pressure your bladder has to exert to empty completely. Another catheter with a pressure-measuring sensor is placed in the rectum or, for women, inthe vagina. During this test, your doctor uses a thin tube (catheter) to fill your bladder slowly with warm fluid. Cystometry is a test that measures pressure in your bladder and in the surrounding region as your bladder fills. A uroflowmeter catches and measures the urine, and translates the data into a graph of changes in your flow rate. To measure the volume and speed of your voiding, you may be asked to urinate into a device (uroflowmeter).
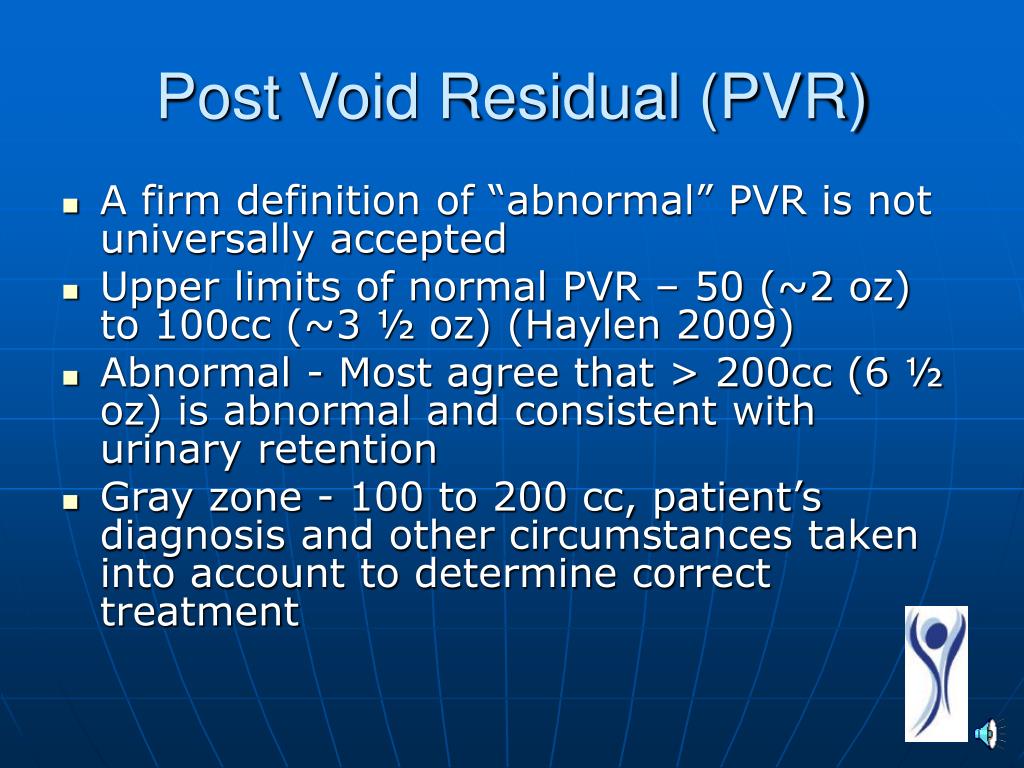
In some cases, a thin tube (catheter) is passed through the urethra and into your bladder to drain the remaining urine, which can then be measured. The ultrasound scan translates sound waves into an image, showing how much urine is left in your bladder after you urinate. To measure residual urine after you have voided, your doctor may request an ultrasound scan of your bladder. Remaining urine in the bladder (post-void residual urine) may cause symptoms identical to those of an overactive bladder. This test is important if there's concern about your ability to empty your bladder completely when you urinate. These tests usually require a referral to a specialist, but testing may not be necessary to make a diagnosis or begin treatment. Your provider may recommend tests to assess how well your bladder is functioning and its ability to empty steadily and completely (urodynamic tests). Focused neurological exam that may identify sensory issues or reflex problems.Urine sample to test for infection, traces of blood or other abnormalities.Physical exam, which may include a rectal exam and a pelvic exam in women.


 0 kommentar(er)
0 kommentar(er)
